Patient safety solutions from experts who understand the challenges you face.
ORDx+Rx: Solutions for Surgical Safety brings together eight renowned physicians, nurses and healthcare quality experts with extensive interdisciplinary experience in patient safety, perioperative and surgical procedure, regulatory requirements, leadership, efficiency, teamwork and department management. We work together with your medical, nursing, technical and administrative teams to improve quality, patient safety and efficiency in your operating rooms and throughout the perioperative process. Restructuring and reorganization of departmental functions is also a necessity in the delivery of quality care. We can help achieve this.
You understand that three disciplines, surgery, anesthesia, and nursing,
must function seamlessly together in operating rooms.
We understand how they can.
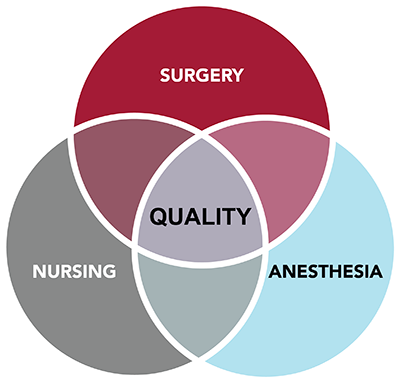
When one or more of these disciplines isn’t healthy, your entire perioperative process is infected – and patients are at risk. ORDx+Rx offers solutions from the world’s top surgeons, anaesthesiologists and nurses – real practitioners who’ve worked in real hospitals caring for real patients.
The ORDx+Rx Difference
We’ve worked in and led operating rooms and departments. Run them. Set the standards for them.
“Rarely have we had the opportunity to work with a group of ORDx’s caliber and reputation ..."
Chief of Surgery, ORDx+Rx Client
The expertise and caliber of our team of experts and our focus on perioperative safety and quality sets us apart. Nowhere in the healthcare consulting world can you find the combined experience and level of expertise that ORDx+Rx will bring to your healthcare organization. When you hire ORDx+Rx, you’ll find hospital board members, past Presidents of the American College of Surgeons, the American Society of Anesthesiologists and the Association of periOperative Registered Nurses, as well as national leaders in quality improvement, working together with you in your operating rooms and perioperative programs.
And nowhere in the healthcare consulting industry will you find a similar focus on patient outcomes and perioperative safety. We understand the reality of healthcare today: your hospital (and your department) is a business, and your operating rooms are the executive boardrooms of that business. But we believe that assessing financial efficiency alone is treating the symptom, not the disease. And you understand that while healthcare is a business, it is the business of providing the best possible patient care. To do that, your department, operating room and the surgical team must function efficiently and effectively – with quality, safety and safe surgical procedures as the foundation.
"... We have seen amazing results in just a few months."
ORDx+Rx Client
How We Work
ORDx+Rx: Operating room diagnosis + prescriptions for quality, efficiency and safety.
We:
- Provide a detailed request for information to prepare for a site visit depending on your needs.
- Meet with your medical, nursing, technical and administrative staff onsite.
- Inspect hospital and facility standards, files, charts, quality reports and critical incident reports. If departmental restructuring is necessary, additional information may need to be gathered.
- Listen carefully and observe practices, flow, facilities and equipment.
- Discuss our findings as a team.
- Convey preliminary observations in an exit conference.
The ORDx+Rx team then prepares an extensive confidential report containing a thorough analysis and specific recommendations. We don’t just drop the report on your desk – our team continues to assist with any correction processes, and we follow up with telephone conferences to assist with implementation. We can tailor our services to fit your needs, and offer add-on services like hands-on implementation and personalized educational webinars that your surgical team can view on demand whenever they’d like.
Our mission is to change these numbers:
“It’s time for Americans to make clear to hospitals that they must earn our business, and our trust, and we will not pay with our lives for their failure to act.”

